Ever have to untangle a knotted ball of yarn? That’s what understanding Medicare costs can feel like. With its mix of premiums, deductibles, copayments, and coinsurance – it’s enough to make your head spin.
I feel ya; I’ve experienced that same confusion. The maze-like nature of this system leaves many overwhelmed and confused. But don’t worry – you’re not alone in this journey.
This post is the flashlight that’ll help illuminate your path through the Medicare labyrinth. We’ll break down complex terms like Income-Related Monthly Adjustment Amounts (IRMAA), shed light on Medicare Advantage plans’ cost structure, explore quality ratings’ impact on costs, and even offer strategies for managing your overall expenses.
So what’s the upshot? You get a crystal-clear picture of Medicare costs, letting you make smart decisions about your healthcare.
Understanding Medicare Costs
If you’re navigating the complex waters of healthcare retirement planning, it’s crucial to get a handle on these costs. Deciphering the Medicare-related terms – premiums, deductibles, copayments and coinsurance – is essential for effective retirement healthcare planning.
Premiums
The premium is the monthly amount you pay for your health care coverage. It varies based on factors such as work history and part B costs. This payment helps secure quality care services like doctor visits or hospital stays.
Deductibles
A deductible is what you must shell out before your plan starts covering benefits. For example, with Original Medicare (Part A), there may be a cost associated with each benefit period in a hospital stay.
Copayments and Coinsurance
Once the deductible has been met, copayments or coinsurances come into play. Copayment is a specific dollar amount paid for supplies or services like eye exams or oxygen tanks for home use, while coinsurance represents percentage-based payments often seen in Part B covers doctor visits, outpatient procedures, and other medical service needs.
| Type of Cost Sharing | Description |
|---|---|
| Premiums: | The monthly fee that secures access to insurance Medicare health coverage options, including covered services under original Medicare or advantage plans, among others, depending on one’s health needs. |
| Deductible: | This initial out-of-pocket expense, which once met, triggers plan members’ eligibility for coverage pay from their chosen Medicare Plan – whether it be an Advantage Plan offering additional prescription drug coverage options or the traditional Medicare Parts A and B. |
| Copayments & Coinsurance: | Extra charges you’ve got to cover once your deductible is met. A copayment is a set cash amount, whereas coinsurance represents a percentage of the expense for each insured service – this could be anything from lab tests at the hospital, seeing your doctor, or getting prescription drugs. |
Key Takeaway:
Getting a grip on Medicare costs is vital for healthcare retirement planning. Here’s the lowdown: you pay premiums monthly, which vary based on factors like work history and Part B costs. Deductibles are what you pay before your plan kicks in, while copayments or coinsurances are extra charges after meeting deductibles.
Navigating IRMAA and Your Medicare Costs
When it comes to managing your Medicare costs, understanding the role of Income-Related Monthly Adjustment Amounts (IRMAA) is crucial. If you’re a wealthier Medicare beneficiary, this could affect you.
Let’s break down what IRMAA really means for your wallet. Essentially, if your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above certain limits (source), then yes – Uncle Sam says it’s time to pay more.
The Impact of IRMAA on Part B Premiums
If you’re part of that higher-income group, both Part B premiums and prescription drug coverage (Part D) can get affected by IRMAA. Here’s how: say you have an individual annual income over $97k or joint incomes over $194k? You might find yourself shelling out up to about $78-$472 extra per month just for Part B & D premiums alone due to IRMAA adjustments.
Mitigating the Effects of Higher-Income Beneficiary Status
But don’t fret. Just because we earn more doesn’t mean our retirement funds should drain faster than a hot tub with a hole in it. A bit surprised? Let me share some tactics I’ve picked up while navigating these murky waters:
- Avoid sudden increases in income: This might sound counter-intuitive, but sudden spikes in income can push you into a higher IRMAA bracket. Consider spreading out large withdrawals from retirement accounts over several years.
- Consider Roth conversions: While this will increase your taxable income in the short term, it could help keep your modified adjusted gross income below the threshold for IRMAA charges in future years.
- Talk to a professional: An experienced financial planner or tax advisor can provide strategies tailored to your specific situation. It’s like having an expert co-pilot navigating with you.
Wrapping it up, getting a grip on IRMAA is key.
Key Takeaway:
Understanding Income-Related Monthly Adjustment Amounts (IRMAA) can be a game-changer in managing your Medicare costs. If you’re high-income, you may need to pay more for Part B premiums and prescription drug coverage. But don’t panic. Tactics like avoiding sudden income increases, considering Roth conversions, or seeking expert advice can help navigate these extra charges.
Table of Contents:
- Understanding Medicare Costs
- Navigating IRMAA and Your Medicare Costs
- The Cost Structure of Medicare Advantage Plans
- Quality Ratings and Their Impact on Medicare Costs
- Decoding Cost-Sharing in Medicare
- The Role of Out-of-Pocket Limits in Controlling Your Medicare Costs
- Strategies for Managing Your Overall Medicare Costs
- FAQs in Relation to Medicare Cost
- Conclusion
The Cost Structure of Medicare Advantage Plans
Medicare Advantage plans, also known as Part C, have a unique cost structure that sets them apart from Original Medicare. Let’s delve into what makes these plans tick.
What are the Key Highlights for 2023 Medicare Advantage Plans?
This year, there’s good news for enrollees in Medicare Advantage Plan Premiums. A whopping 73% pay no premium other than their Part B premium. This means they get to enjoy more benefits without any extra costs.
Out-of-pocket limits can significantly impact the total cost of healthcare for any given year, making them an important factor to consider. In-network services come with an average out-of-pocket limit of $4,835 this year. For both in-network and out-of-network services combined, it stands at $8,659 on average.
How Do Premiums for Medicare Advantage Enrollees Compare to Previous Years?
If we look back at the history of plan premiums over the years and compare them with today’s rates – well let me tell you – our current position isn’t half bad. With time we’ve seen substantial growth in value-added supplemental benefits offered by these advantage plans while keeping your pocket strain surprisingly manageable.
In fact when it comes down to doctor visits or even outpatient procedures under part b covers – most people enrolled find themselves enjoying medical service without feeling financially overwhelmed which is always great news.
Note: You should not assume that lower cost equals lesser care quality. It is possible due to factors like provider networks negotiations and utilization management techniques.
Additionally, many Medicare Advantage plans offer additional benefits such as prescription drug coverage and eye exams or hospital lab services that may not be covered under Original Medicare – something to consider when evaluating your health needs. These often include things like eye exams or even hospital lab services – aspects not always covered under Original Medicare. So it’s worth considering if these perks are essential for your health needs before making a choice.
Wrapping up, getting the hang of Medicare Advantage Plans’ cost structure is key.
Key Takeaway:
Good news for those enrolling in Medicare Advantage, or Part C, plans in 2023 – nearly 73% won’t pay any extra premium beyond their Part B. The average out-of-pocket limit sits at $4,835 for in-network services and caps off at a combined total of $8,659. Despite more value-added benefits popping up over the years, costs have stayed put.
Quality Ratings and Their Impact on Medicare Costs
Did you know that the quality of your Medicare plan can have a significant impact on your healthcare costs? It’s true. Let me explain how it works.
The Centers for Medicare & Medicaid Services (CMS) uses a star rating system to evaluate the performance of various plans. According to the CMS Fact Sheet on 2023 Medicare Star Ratings, most enrollees are in plans with a quality rating of at least 4 out of 5 stars. That’s quite reassuring, isn’t it?
This means they’re enrolled in high-quality plans which not only meet but often exceed standard requirements for coverage and service delivery. However, this doesn’t mean higher ratings always translate into lower costs.
Racial Disparities Influence Plan Quality
It’s important to consider factors like racial disparities when looking at these ratings. An enlightening piece from Health Affairs reveals some unsettling truths about racial disparities and quality improvement. In certain cases, beneficiaries from racially diverse backgrounds might find themselves facing different experiences compared to their counterparts despite being under the same rated plan.
The Role Of The Quality Bonus Program
You might be wondering now – what incentivizes insurers to aim for higher ratings? Well, enter CMS’ Quality Bonus Program. A well-researched article by Health Affairs sheds light on this bonus program designed by CMS. Insurers with higher-rated plans are rewarded financially, which encourages them to continuously improve their services. In theory, this should result in better care for enrollees.
However, this does not guarantee a straightforward improvement in care for enrollees. A crucial stat reveals that nearly all (99%) of these highly rated plans require prior authorization for some services. This means you may need approval before getting certain types of care or medications covered.
Prior Authorization Can Impact Costs
So, remember that prior authorizations might bump up your Medicare costs. They could hold back needed treatment and cause extra out-of-pocket expenses if the ask is turned down. High star ratings look great on paper, but personal experiences can vary.
Key Takeaway:
Understanding the impact of quality ratings on Medicare costs is key. The Centers for Medicare & Medicaid Services uses a star system to rate plans, with most enrollees in 4-star or higher programs. But remember, high ratings don’t always mean lower costs due to factors like racial disparities and prior authorization requirements.
Decoding Cost-Sharing in Medicare
When attempting to figure out the costs associated with Medicare, it is important to comprehend the cost-sharing details. This includes coinsurance, copayments, and deductibles.
Understanding Coinsurance
In essence, coinsurance is the percentage of medical service costs that you have to pay after meeting your deductible. So if your plan has a 20% coinsurance rate for doctor visits or hospital lab services covered by Medicare Part B, this means that once you’ve met your deductible, you’ll be responsible for paying 20% of these healthcare expenses while Medicare pays the remaining 80%. The key takeaway? Your actual out-of-pocket costs can vary depending on how much care you need.
The Role of Copayments
Copayment functions differently from coinsurance as it is not dependent on percentages but rather specific dollar amounts assigned per service type. For instance, with some prescription drugs under part D IRMAA or during an outpatient procedure visit – instead of having variable charges based on total medication cost or surgical fees – there might be a fixed co-pay amount such as $15 per drug prescription filled or $50 per doctor visit irrespective of overall treatment expense.
Deductible Dynamics
Your annual deductible represents what comes out-of-your-pocket before coverage kicks in fully. Whether we talk about original Medicare (Part A & B) premiums and benefits provided under them like eye exams and oxygen tanks supply at home – they all start offering their maximum benefit only post hitting this threshold limit defined annually by CMS (Centers for Medicare & Medicaid Services). After you have met your annual deductible of $200, any remaining costs for doctor visits, such as the $50 in this example, will be subject to coinsurance or copayment.
Cost-sharing mechanisms in Medicare are designed to keep healthcare costs manageable while also encouraging responsible usage of medical services. By understanding how these elements work together – from co-pays for prescription drugs under part D IRMAA to deductibles associated with original Medicare plans – beneficiaries can make more informed decisions about their health care services leading to securing quality care without breaking the bank.
Key Takeaway:
Understanding the ins and outs of Medicare’s cost-sharing features such as coinsurance, copayments, and deductibles is crucial to keeping your healthcare costs in check. Coinsurance has you paying a share of medical bills after hitting your deductible; copayments are fixed fees per service type; while the deductible is what you fork out before full coverage kicks in. Getting to grips with these elements – from Part
The Role of Out-of-Pocket Limits in Controlling Your Medicare Costs
When it comes to controlling your healthcare expenses, understanding the role of out-of-pocket limits can be a game changer. These limits cap the amount you have to spend on health care services during a plan year.
In Original Medicare and Medicare Advantage plans, out-of-pocket costs encompass deductibles, copays, and coinsurance for eligible services. But here’s where they differ: unlike Original Medicare, most Medicare Advantage plans set an annual limit on what you pay out of pocket.
In-Network Services vs Out-of-Network Services
The distinction between in-network and out-of-network services is crucial when talking about these limits. In-network refers to providers or health-care facilities that are part of a health plan’s network. Typically, insurers negotiate lower rates with these providers – making them less costly than those outside the network.
Most people know this but many overlook how it impacts their total healthcare bill at the end of each year because they don’t realize there may be separate caps for these types of service.
Capping Your Medicare Costs Can Save You Money
Spoiler alert: This can save you some serious cash. The beauty lies within its simplicity – once you reach your out-of-pocket maximums (caps), any further covered medical service costs will be handled by your insurance company under terms specified in your policy.
You might think hitting that limit would require frequent doctor visits or expensive procedures but actually everyday items like prescription drugs, eye exams or even hospital stays can quickly add up. It’s like having a safety net for your health expenses.
Planning and Vigilance are Key
To effectively use out-of-pocket limits as a cost control tool, it’s important to keep track of your medical spending throughout the year. This involves keeping an eye on how close you’re getting to that limit – consider it akin to checking your car’s gas gauge during a road trip.
You might find it helpful to ask questions about all potential costs before receiving care services or choosing coverage options, especially when dealing with providers outside the network.
Key Takeaway:
Knowing your Medicare out-of-pocket limits is like finding a secret weapon for controlling healthcare costs. It’s the cap on what you shell out each year, and once reached, your insurer steps in to cover further expenses. Keep track of those dollars spent and be mindful when choosing between in-network or out-of-network services – it can save you big time.
Strategies for Managing Your Overall Medicare Costs
Gaining a comprehensive understanding of your Medicare coverage can empower you to control your healthcare costs.
How Can You Maximize Your Medicare Benefits?
You can maximize your benefits by making smart use of preventive services. Regular health checks help catch potential issues early when they’re often easier (and cheaper) to treat. Most importantly, many preventive services, such as cancer screenings and flu shots, are covered under both Original Medicare and most Advantage Plans at no extra cost.
To further manage expenses, consider sticking with in-network providers whenever possible. Sticking with in-network providers will help you get the most out of your plan and keep costs low.
What Are Some Effective Ways To Manage Prescription Drug Costs?
Good news for those whose prescription drugs make up a large part of their healthcare costs. There are strategies available to help lower these costs. One way is through exploring Medicare’s Extra Help program. It provides assistance for people with limited resources who need help paying Part D premiums or other drug-related costs.
You may also want to ask if generic versions of expensive brand-name drugs exist because generics usually cost less but work just as well.
Additionally, using mail-order pharmacies could save money on long-term prescriptions because they typically offer larger quantities at lower prices than traditional pharmacies do.
Lastly, always keep an eye on the coverage options offered by different Medicare plans. Every year during open enrollment, you have a chance to switch plans if another one offers better cost-saving opportunities for your specific needs.
In summary, managing healthcare costs doesn’t need to be daunting. By utilizing preventive services and choosing in-network providers where possible, as well as effectively managing prescription drug costs and exploring Medicare’s cost-saving programs, you can navigate through your golden years without breaking the bank.
Key Takeaway:
Knowing your Medicare coverage well helps keep costs down. Make smart use of preventive services and stick with in-network providers to maximize benefits while minimizing expenses. For managing prescription drug costs, explore programs like Extra Help, consider generics, use mail-order pharmacies for long-term prescriptions, and regularly review plan options during open enrollment.
FAQs in Relation to Medicare Costs
How much are Medicare costs each month?
The monthly Medicare Part B premium for 2023 is $164.90 on average, but it can vary based on your income.
What does Medicare A and B cost per month?
In general, most people don’t pay a Part A premium, while the standard Part B premium in 2023 is $164.90.
What are Medicare costs per month in 2023?
The average monthly cost for Part D drug plans varies widely by plan, adding to the standard Parts A & B costs.
How much is taken out of Social Security for Medicare in 2023?
If you get Social Security benefits, the standard Part B premium amount will be usually deducted from your benefit payment.
Conclusion
Decoding the complexities of Medicare costs, you now have a roadmap to navigate premiums, deductibles, copayments, and coinsurance. It’s about understanding the pieces that form your healthcare puzzle.
You’ve grasped how Income-Related Monthly Adjustment Amounts (IRMAA) can sway your overall costs. You’ve delved into Medicare Advantage plans’ structure – with their out-of-pocket limits and supplemental benefits – seeing how they compare against traditional Medicare.
You’ve discovered quality ratings’ impact on expenses while unraveling cost-sharing mechanisms like coinsurance and copayments. And finally, learned about strategies for managing prescription drug costs and utilizing preventive services.
All this knowledge empowers you to make smart decisions about your health coverage options because at the end of it all – it’s not just about getting care; it’s also securing quality care without breaking the bank.
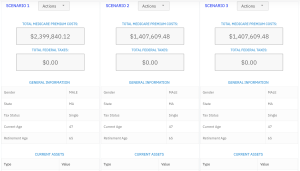
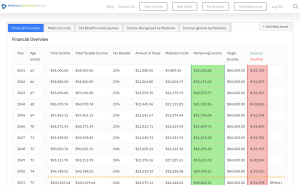
Streamlining the Medicare Surcharge Calculation Process.
Our Healthcare Retirement Planner software is designed to streamline the retirement planning process for financial professionals. By providing an efficient way to calculate IRMAA costs, our tool helps you save time and focus on other aspects of your clients’ retirement plans.
- Faster calculations: Our software quickly calculates IRMAA costs based on your client’s income and tax filing status, eliminating manual calculations and potential errors.
- User-friendly interface: The intuitive design of our platform makes it easy for financial professionals to input data and generate results with minimal effort.
- Data integration: Seamlessly integrate our calculator into your existing financial planning tools or CRM systems for a more streamlined workflow.
- Easy to Understand Reports: Export reports to easily share with your clients
- Tax and Surcharge Modeling: see how different types of income affects both taxes and your surcharges.
In addition to simplifying the calculation process, using our Healthcare Retirement Planner can also help improve communication between you and your clients. With clear visuals that illustrate how IRMAA costs impact their overall retirement plan, you can effectively convey complex information in an easily digestible format. This enables clients to make informed decisions about their healthcare expenses during retirement while ensuring they are prepared for any potential changes in Medicare premiums due to income fluctuations. To learn more about how our software can benefit both you as a financial professional and your clients’ retirement planning experience, visit the features page. Streamlining retirement planning processes can help financial professionals save time and resources, allowing them to focus on other areas of their clients’ needs. Automated calculation of IRMAA costs is the next step in streamlining this process even further.